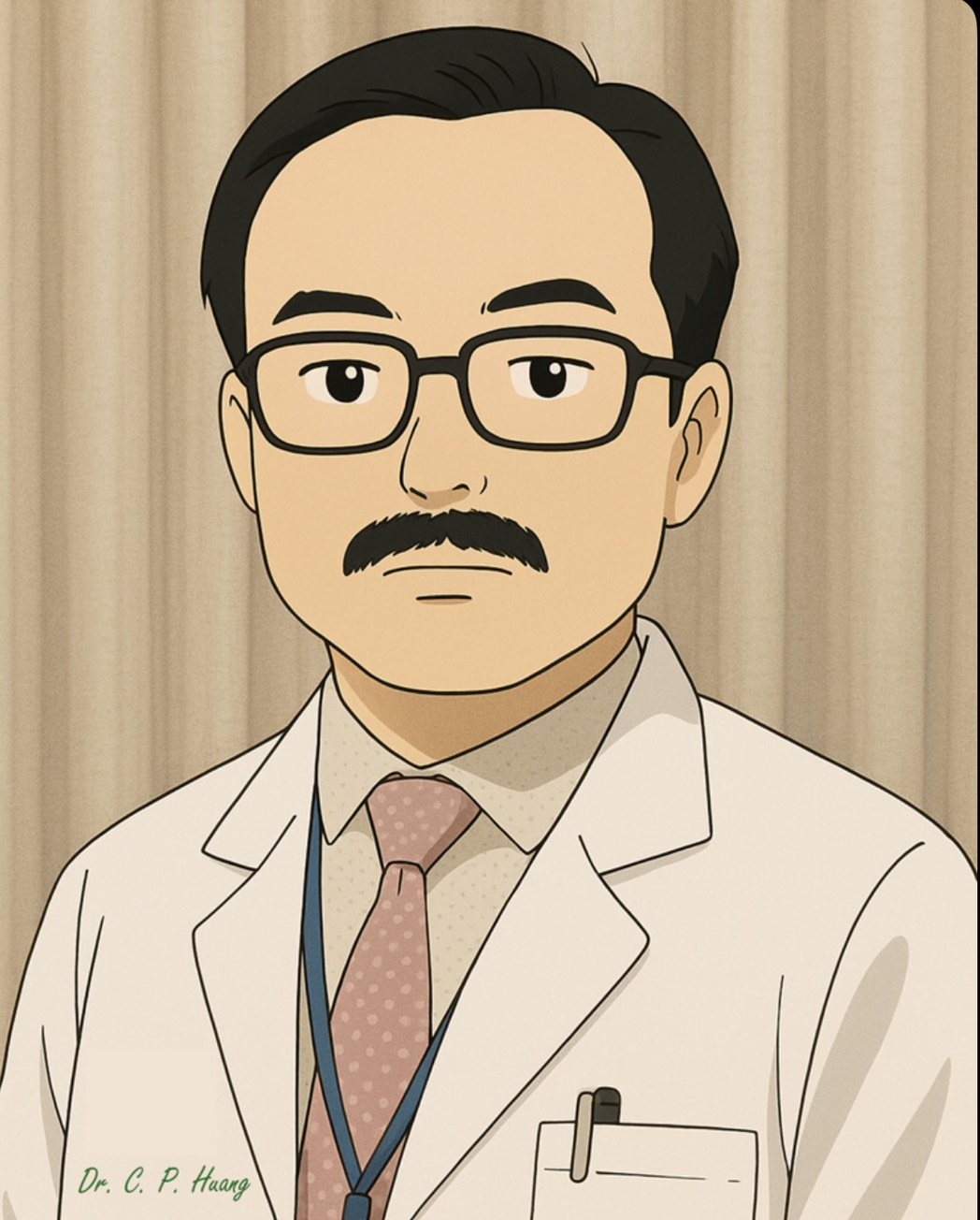
Chi-Ping Huang
Dr. Chi-Ping Huang worked as the director of the Department of Urology in CMUH. His specialties include the diagnosis and treatment of urological malignancy (such as prostate cancer, kidney cancer, bladder cancer, and ureter cancer), minimally invasive surgery, and kidney transplantation. Dr. Huang has many experiences in performing surgeries using the daVinCi robotic surgery system and has accumulated over thousands cases. He had received training courses of robotic-surgery at the Ohio State University Medical Center in the United States. He also had training courses of kidney transplantation at the Tokyo Women's Medical University Hospital in Japan. He is also skilled in performing minimally invasive surgery for benign prostatic hyperplasia and cell immunotherapy for urological cancers.
15th August 2025
| Time | Session |
|---|---|
|
13:30
15:00
|
Renal Cell Carcinoma
TICC - 2F 201BC
|
|
15:30
17:00
|
Oncology RCC (A)
Cheryn SongKorea (Republic of)
Moderator
Assistance of the AI during RAPN - Surgical Navigation to Outcome PredictionArtificial Intelligence (AI) has deeply infiltrated many, if not every, aspects of our lives - both professional and ordinary corners. In medicine, it seems that any research dealing with large amounts of data has to employ AI in one way or another - from radiomics and radiogenomics to drug developments and simulations. In managing patients with renal tumors, majority of which now present with localized, small masses, I have focused on developing a tool to help establish a plan preoperatively and navigate throughout the surgery, in real-time with the help of the AI. Using kidney dynamic CT scans of 100 patients undergoing robot-assisted partial nephrectomy, software was developed to render a 3-dimensional image of the kidney harboring the tumor along with several other tools to enhance visualization of the lesion. Scans from an additional 30 patients were used to test for performance and validate the software. Before surgery, main renal pedicles, tumor location with respect to the major hilar vasculature, important landmarks including the calyces and branches of the vessels can be studied from all angles; tumor shape especially when it is not a perfect sphere can be visually presented and the excision of the tumor with desired margin thickness can be simulated to see what vital structures come into contact. Connected to the surgeon console through the TilePro® screen, it was designed to aid a urologic surgeon from before surgery as well as throughout the procedure as needed. In a phase I feasibility trial investigating the efficacy of the system, we confirmed that the integration of the 3D navigation system into RAPN was both feasible and safe, providing enhanced anatomical information while maintaining a consistent level of operative risk. The use of navigation system resulted in reduced renal parenchymal volume resected, suggesting potential benefits in renal function preservation. Subsequent phase 2 trial investigating accuracy of the reconstruction and a multicenter randomized controlled trial with surgeons with varying degrees of experience are underway to validate the benefits.
On the other hand, the fundamental question as to best manage the small renal masses – i.e. indications for partial nephrectomies - still harbor some gray areas: is partial nephrectomy at all possible situations the best? In a given patient how will oncological and renal functional outcome differ between partial and radical nephrectomy? Previous statistical methods could only calculate risk ratios in the best-matched cohorts and the issue of counterfactual remained. Using demographic and tumor descriptive parameters of 1,448 patients with pT1N0M0 RCC patients from three academic centers, causal inference was modeled using a double machine learning algorithm to predict progression-free survival and eGFR at five years according to each surgical method: partial and radical nephrectomy. We identified significant factors and their contribution to the outcomes of interest to be included in the model. Selecting a model with the highest performance among various machine learning models for each outcome, an online interface was constructed. External validation confirmed the robustness, presenting AUROC of 0.758, AUPRC of 0.200 with XGBoost model for recurrence, and RMSE of 15.9 with GBM model for eGFR. By presenting numerical predictions of oncologic and functional outcomes associated with partial and radical nephrectomy in a given patient, our model facilitates individualized, evidence-based clinical decision-making.
TICC - 1F 101D
|